The following is our "On the Record" information that was sent to The New York Times reporters before publication of the latest installment of its series on Catholic healthcare.
Also, you can learn about some of the heroic work of our caregivers by watching this video.
***
Thank you for giving us the opportunity to respond to the latest installment of your healthcare series targeting Catholic health systems.
Ascension is deeply committed to providing a positive workplace culture for our nurses, as well as other clinicians and associates. Doing so is not only an inherent aspect of valuing the dignity of our colleagues, but a well-functioning and supported workforce improves the quality of care we provide to the communities we serve. Unlike what The New York Times has indicated that it was told, the reality is that Ascension’s hospital staffing levels – particularly bedside nursing staffing – increased in the years leading up to the pandemic and continue to exceed levels maintained by the majority of our peers.
Ascension is also committed to continually measuring and improving the quality of care provided to the communities we serve. Despite facing unprecedented and challenging financial times, our dedication to our Mission is evidenced by the fact that we provided nearly $2.3 billion in care of persons living in poverty and other community benefit programs during our last fiscal year ended June 30, 2022. Since fiscal year 2010, Ascension has provided more than $23.5 billion in care of persons living in poverty and community benefit.
Quality/Patient Safety
Our commitment to maintaining a strong and resilient workforce arises out of our dedication to providing quality care for our patients, our Mission, and our Values. Ascension is deeply committed to continually measuring and improving the quality of care provided to our patients. Ascension’s clinical quality is excellent overall, exceeds that of our peers across multiple key metrics, and has been improving over time.
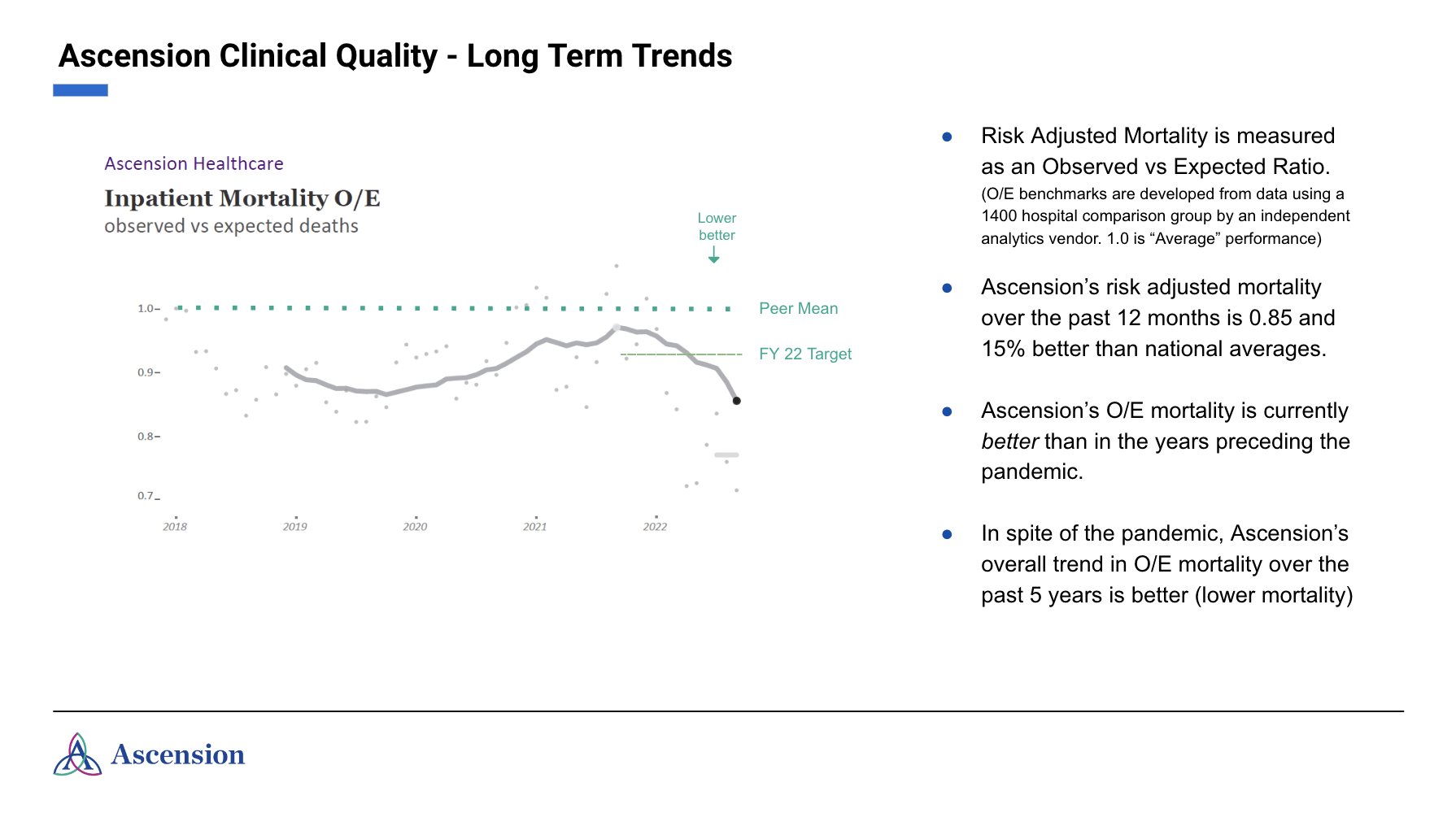
For instance, in terms of clinical outcomes, Ascension’s system-wide risk-adjusted mortality has shown improvement over many years and is currently at the lowest level measured in seven years. While many hospitals and health systems saw an increase in mortality during the COVID-19 pandemic, Ascension’s system mortality results are better than two-thirds of hospitals measured nationwide. During the COVID-19 pandemic, Ascension placed significant focus on taking a consistent, system-led approach to managing COVID-19 infection. Our efforts have been directly associated with better outcomes; our risk-adjusted mortality over the past 12 months is 15% better than the national comparator group. See Table 1.
Table 1.
Another important indicator of quality of care delivered is the risk-adjusted readmission rate, which is an indicator of properly completing care and preparing patients to continue their recovery outside of the hospital setting. Ascension’s System-wide risk-adjusted readmission rate is 6% lower (better) than the national average.
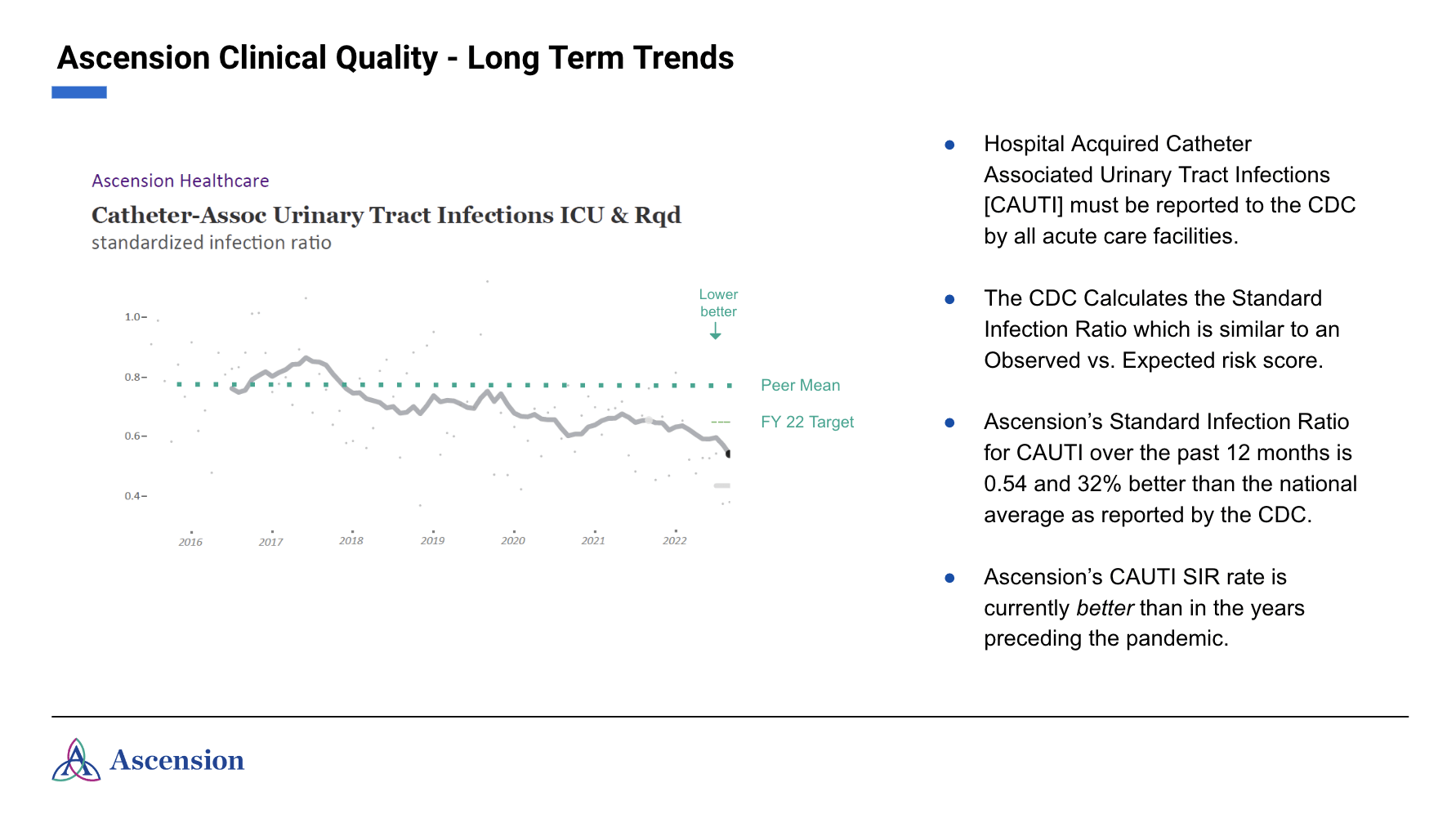
Quality measures related to infection rates are also significantly better at Ascension than the national average. Importantly, these represent nursing-sensitive measures, meaning our outcomes are directly influenced by nursing care. Two recognized indicators of strong nursing performance relate to infections from central lines and the use of urinary catheters. Ascension’s central line associated bloodstream infections over the past 12 months are 21% lower than the 2021 CDC reported national performance; urinary catheter associated infections are 32% lower than the national performance over the same period. See Tables 2 and 3. In addition, hospital pressure ulcer complication rates have been well below the national average and are currently 36% below the national average rate as observed by a typical hospital.
Ascension’s commitment to its nursing staff and quality patient care are reflected in these strong outcomes.
Table 2.
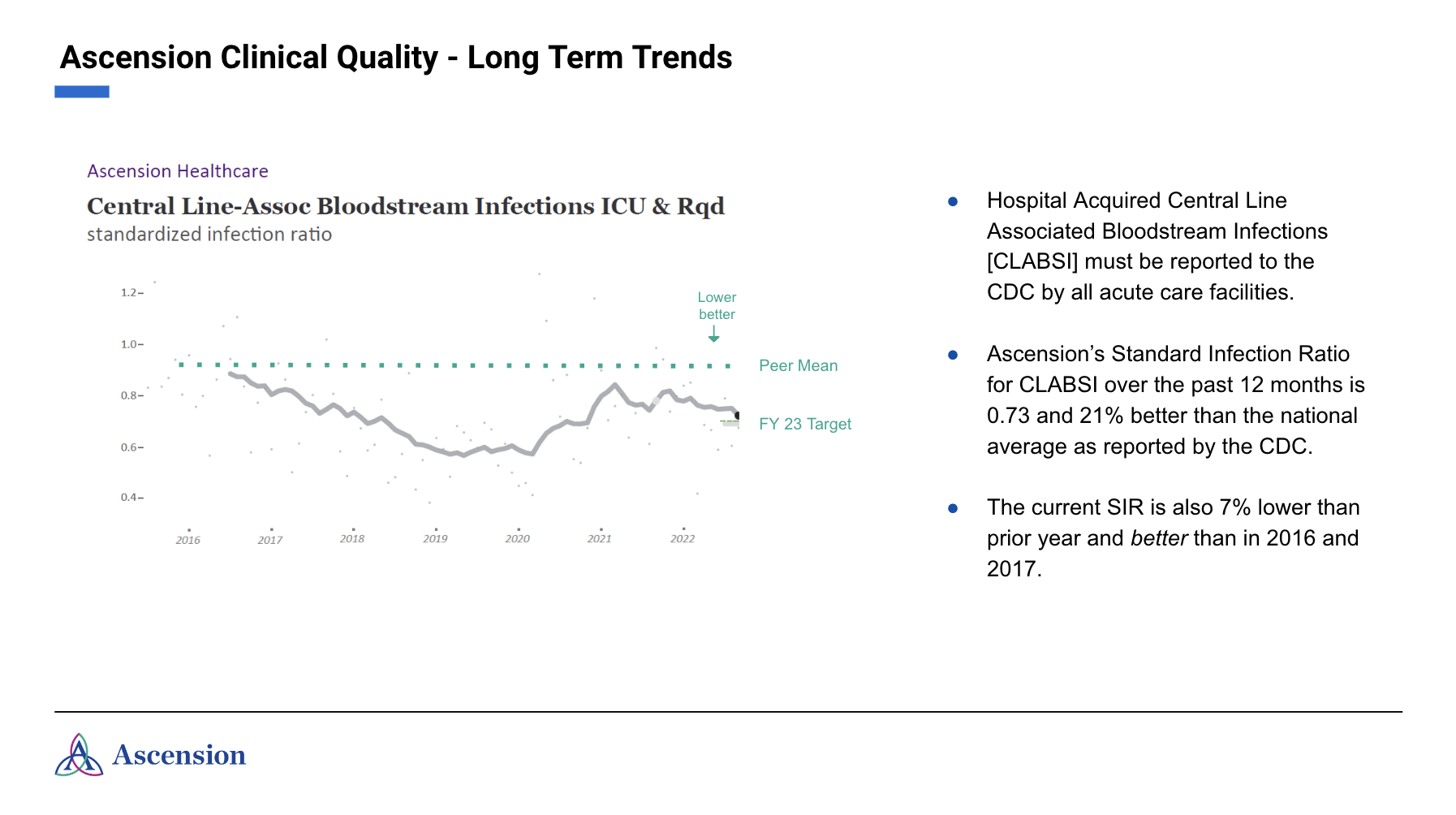
Table 3.
Growth in Staffing
In addition to the efforts we have made in support of our workforce and to maintain and improve the quality of care provided during COVID, our commitment to maintaining a strong workforce extends well beyond the pandemic years. Overall staffing across Ascension increased from 82,334 full-time equivalent (FTE) employees in fiscal year 2010 to 124,995 FTEs in the fiscal year ended June 30, 2020, at the start of the COVID-19 pandemic. This growth was consistent throughout the period around 2012 when our operating model began moving from a holding company to an operating company. This change improved our operational efficiency by consolidating and streamlining back-office functions in the areas of human resources, supply chain, finance and related business functions so that we could direct more of our resources to patient care and clinical staffing.
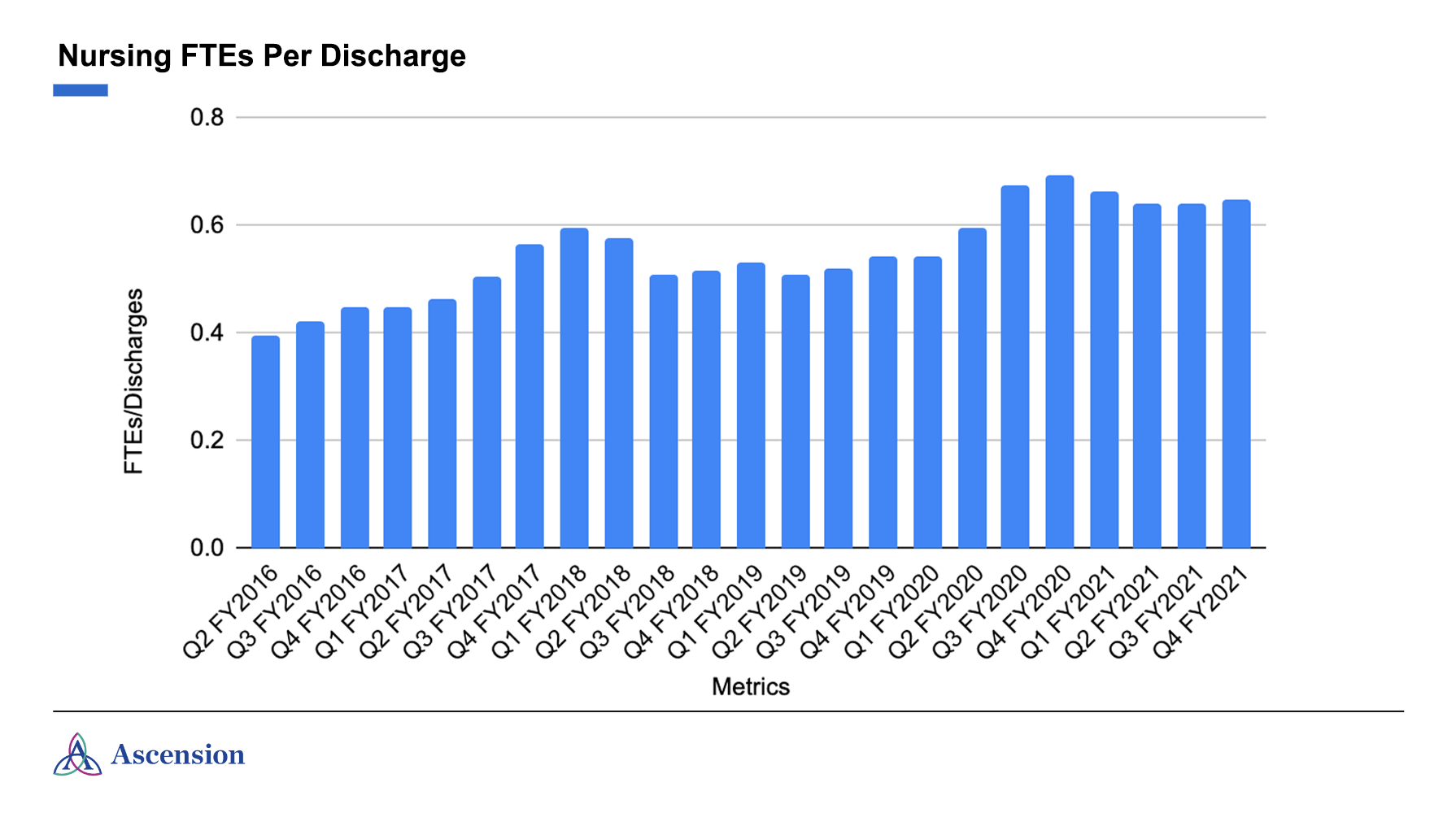
Similarly, the number of bedside nurses at Ascension hospitals has increased, particularly in the years leading up to the pandemic. From 2016 to the present, the number of bedside nursing FTEs per patient discharge has increased 64% while the number of discharges has remained relatively flat. See Table 4.(1)
Table 4.
Furthermore, independent third-party analysis by Accenture demonstrates that our staffing levels overall exceed those consistently maintained by our peers – with our Michigan market most significantly exceeding comparable industry benchmarks. From 2013-2021, Ascension Genesys’ level of nurse staffing far exceeded the state of Michigan median. In fact, Ascension Michigan’s hospitals overall exceeded the median. In Illinois, our hospitals had staffing levels comparable to their peers, yet while other systems’ nursing numbers are falling, Ascension Illinois’ are growing, and our nurse staffing exceeded the median in 2021, the most recent year that data is available.
For FY2021, according to Healthcare Management Partners, which uses the Centers for Medicare & Medicaid Services cost report database, Ascension Genesys FTEs per Adjusted Occupied Bed (AOB) was 5.82, which was above the market benchmark, and at Ascension Saint Joseph in Joliet, FTEs per AOB was 5.02, which was also above the benchmark for peers in that market. While benchmark numbers have not been published for FY2022, we have no reason to believe that we have fallen below the market benchmark in either market for that time frame. We shared that the ratio of FTEs per AOB at Ascension Genesys was 5.07 in FY2018. It increased in years that followed and was 5.67 in FY2021, which was during the pandemic, and the most recent year that data is available. The ratio for Ascension Genesys has continued to increase over time and is effectively in line with the FY2021 5.82 ratio for peer hospitals in the Michigan market.
Also, the ratio of FTEs per AOB at Ascension Saint Joseph in Joliet was 4.72 in FY2018. This ratio also increased in years that followed and was 5.02 in FY2021, during the pandemic, and the most recent year that data is available. The ratio for Ascension Saint Joseph has continued to increase over the timespan covered by the story and is effectively in line with the FY2021 4.92 FTE per AOB ratio for that market. We also shared that the market benchmarks for Ascension Genesys include data from hospitals in Flint, Michigan, and the market benchmark for Ascension Saint Joseph in Joliet includes data from hospitals in the Core Based Statistical Areas (CBSAs) for Chicago-Naperville-Arlington Heights, Illinois, Kankakee, Illinois, and Elgin, Illinois. In both cases it includes data from both nonprofit and for-profit hospitals where applicable.
We shared our nursing FTEs per discharge figures from across the System to provide an overall view of nurse staffing levels across our footprint, while the data on FTEs per AOB was provided for Ascension Saint Joseph in Joliet, Illinois, and Ascension Genesys in Grand Blanc, Michigan, as this is the standard metric for benchmarking staffing levels in comparison to peers. The calculation of FTE per AOB reflects all patient volumes, including admissions and outpatient volumes. FTEs per AOB is also adjusted for acuity and length of stay to further provide an accurate measure of the staffing provided for patient care needs. Discharge data provided was with respect to the settings noted above and was not adjusted for acuity or length of stay. The result is that the FTE per AOB is a more precise measure of staffing than FTEs per discharge and, thus, why FTEs per AOB is the industry standard. However, the data on the number of FTEs included in both the “FTEs per discharge” metric and the “FTEs per AOB” metric are consistent across both metrics in terms of FTEs attributed to each of these facilities. In other words, the data for FTEs and discharges originate from the same facilities (i.e., the same business units and nested departments) in both the numerator and denominator, and the nursing “FTEs per AOB” provided for Ascension Saint Joseph and Ascension Genesys include the same nursing FTEs attributable specifically to those facilities.
Why There is a Staffing Crisis Now
As a result of investments in staffing and commitment to mission, Ascension had a firm clinical staffing foundation coming into the pandemic, but the global COVID-19 pandemic has had a serious impact on the workforce across all sectors of the economy and especially on the heroic nurses and other caregivers who have been on the front lines of care. The New York Times itself reported in July of this year on how the “chronic nursing shortage is worsening.” Any allegation that Ascension’s current workforce challenges relate to workforce decisions made in years prior to the COVID-19 pandemic is fundamentally misguided, misleading, and demonstrates a lack of understanding of the impact of COVID-19 on the healthcare workforce.
Instead, it is an unfortunate reality that hospitals across the U.S. are dealing with historic staffing challenges due to ongoing workforce shortages. It is not hyperbole to say that the entire U.S. healthcare system is in crisis, or as Forbes put it, in danger of “crumbling due to staffing shortages.” In a letter sent in March to the House Energy and Commerce Committee, the American Hospital Association called the workforce shortage hospitals were experiencing a “national emergency.” This is due in part to the “great resignation” as a result of the COVID-19 pandemic, leading hospitals to compete for a limited number of nurses and other clinical staff, which has been exacerbated by educational institutions not training enough staff to make up the shortfalls.
According to Lightcast, U.S. job posting demand for registered nurses (RNs) has increased 16% since October 2021. But despite rising demand for RNs, monthly hires have remained relatively flat over the last two years. According to the Advisory Board, the total supply of RNs has decreased by over 100,000 in 2021, the greatest drop in supply seen in four decades. Overall demand for RNs is projected to increase by 9%, which is slightly faster than the average growth rate (8%) for all occupations, yet enrollment in entry-level baccalaureate nursing programs increased by 3.3% in 2021, which is the slowest growth in nursing program enrollment since 2015. This, paired with 91,938 qualified applicants who were denied enrollment, continues to create difficulty for hospitals’ staffing levels.
In a study done earlier this year, the U.S. Bureau of Labor Statistics reported “that more than 275,000 additional nurses are needed from 2020 to 2030.” The study sites several factors for the dearth of nurses, including the aging population causing an increased need for health services; an aging workforce, with more than 1 million RNs currently over 50 years old; nurse burnout, including both new and experienced nurses deciding to leave the profession (nurse turnover rates across the U.S. range from 8.8% to 37%); nurses of childbearing years choosing family over career; and the problem of violence in the healthcare setting, with between 8% and 38% of healthcare workers across the world suffering some form of violence in their careers.
In order to maintain access in service to our communities, Ascension has hired higher-cost contract staff to address the nursing crisis, a solution that is not sustainable for the long term for myriad reasons. We are also investing in our associates – as outlined further below – and offer numerous programs and innovations to promote their well-being.
To advance long-term solutions, we are supporting colleges and allied health programs in efforts to attract more students. Ascension is also focused on creating innovative, sustainable programs that help our entry-level associates gain the skills and knowledge needed to transition into advanced roles. These pipeline programs work with local high schools and underserved communities to build early career programs that further the Mission of Ascension and Catholic healthcare. We employ a team dedicated to connecting with our current associates and have achieved a 96% retention rate by conversing personally with associates and exploring their career aspirations. In those conversations, we focus on offering personalized career development and support. By advocating on behalf of associates and fostering an environment of internal movement, we have seen almost 20,000 associates move into new roles within the organization in 2022. Further, through the creation and launch of the Vocare program (stemming from the latin word “to call”), many of our entry-level associates are eligible for debt-free education. This program creates opportunities for increased compensation, which can have life-changing implications for these associates and their families.
Commitment to Associates
Early in the COVID-19 pandemic, Ascension made a commitment to protect the pay of associates during a time of intense disruption, including a commitment to no layoffs and a variety of pay protection programs. This included continued financial support for those who were temporarily assigned to a different job within the ministry or unable to work because they had been diagnosed with or were suspected of having COVID-19.
In addition, Ascension Critical Staffing Pay (a pay practice designed to recognize associates for working shifts in excess of their FTE status, which facilitates appropriate staffing levels based on fluctuations in patient volumes or acuity) was enhanced and expanded to include all front-line clinical associates working in markets with patient surges. Ascension covered 100 percent of the hotel stay cost for clinical associates who chose to stay in a hotel during the pandemic to eliminate any concern regarding unintentional contamination to their family members and/or who volunteered to serve in a market more than 50 miles from their home. Ascension established a COVID-19 Hardship Financial Assistance Program to help associates experiencing financial hardship as a result of the pandemic. And the ministry provided dependent care support to help ease the financial hardship of unexpected dependent care expenses for elderly and special needs family members and children under age 13. And to support Ascension staff and their families, several executive leaders pledged a portion of their salary as a donation to various established emergency funds.
As noted by Becker’s Hospital Review, Ascension President and CEO Joe Impicciche told associates: “We are blessed to be able to make this commitment and appreciate the tremendous work and flexibility of our associates, leaders and physicians in providing compassionate, personalized care. I am proud to witness the way all associates have come together to address the challenges of today, just like we have throughout our history.”
Associates appreciated Ascension’s commitment to their well-being, sharing feedback including:
- “I am grateful and thankful that [Ascension] St. Vincent has made note to offer pandemic pay if we are canceled from our shift during this time and offer to place staff in a hotel if need arises to be quarantined away from family due to exposure.”
- “Thank you for … all your efforts to help us continue to make our patients’ and associates’ needs and safety a top priority. I am so proud to be part of the Ascension team.”
- “I just read the email you sent regarding the various pay protection programs. So unbelievably generous of Ascension! Thank you!”
Importantly, this pledge was made when our revenue had drastically decreased, and we did not know if or when we would receive any financial support from the federal government. We did not know when elective surgeries would restart. As other hospital systems made difficult but understandable workforce decisions because of the massive accumulation of losses, Ascension provided assurances to associates that helped them focus on the COVID patients they served so well. It is plain and simple: Ascension cares about its associates and the patients they serve.
About Operating Margins and Financial Reserves
Ascension relies on reasonable and customary financial reserves to support our commitment to the communities we serve. Were it not for these reserves, we would not have been able to maintain pay and continued employment for associates at the beginning of the COVID-19 pandemic. Ascension went for months essentially without revenues during this time, and yet has provided quality care to more than 1.25 million COVID patients to date while mobilizing to provide over a million vaccine doses within our communities. Even as consumers became more comfortable accessing healthcare again, our operating margins throughout the ongoing pandemic have been (and continue to be) negative; yet, we continue to serve the poorest and most vulnerable patients in our communities because we maintained vital financial reserves.
We are committed to being good stewards of finite resources. In these times of lean and unpredictable operating margins arising out of government payer mixes and pricing inelasticity (the inability to increase prices to keep pace with inflationary expenses), Ascension strives to maintain a strong balance sheet to support operations through returns on investments, which allows us to responsibly finance necessary infrastructure projects, innovative technologies and quality improvement efforts; maintain our community benefit and charity care offerings; and access lower-interest debt when necessary. All of these investments in turn support our high-functioning workforce and quality care. And above all, during these unprecedented challenging financial times, our dedication to our Mission is evidenced by the fact that we provided nearly $2.3 billion in care of persons living in poverty and other community benefit programs during our last fiscal year ended June 30, 2022.
Historically, Ascension has operated on lean and fluctuating margins, largely resulting from a combination of a heavy governmental payer mix; fixed, and in some cases insufficient, commercial reimbursement rates; and a commitment to care for the uninsured. Hospital operations are a capital-intensive business. Over the last 13 years, Ascension has averaged a relatively small operating margin of only 2.15%, and during our last three fiscal years (the COVID and post recovery period), Ascension has had an average annual operating loss of roughly -1.0%, which is an average annual loss of approximately $280 million and total operational loss of just over $840 million over this three-year period. Even while sustaining those losses, we provided care for a total of 1,277,576 confirmed COVID patients across Ascension as of December 4, 2022 – including inpatient stays, emergency department visits, outpatient care and observation stays. We cared for 163,112 of the sickest of these COVID patients as inpatients in our hospitals and an additional 1,655 frail patients residing in our Ascension Living facilities. We also mobilized across our ministries to provide vaccinations, using mobile vans, mass clinics and direct patient outreach to support the provision of more than one million vaccine doses.
And despite these historically narrow margins, over this same 13-year period, Ascension has maintained its commitment to the poor and vulnerable with an average of $1.8 billion annually in care for the poor and community benefit provided; and during the past three-year period when operating margins were negative, Ascension increased these community contributions to an average of $2.3 billion in care.
It’s important to understand that nonprofit organizations rely on strong balance sheets to provide the flexibility needed to respond to changing conditions and the needs of communities. Our so-called “wealth” does not derive from positive operating margins. Instead, we have built reasonable cash reserves proportionate to our size to supplement our margins, a practice consistently recognized by the bond rating agencies whose favorable ratings directly impact our ability to responsibly finance debt, as discussed below. In addition to supporting our ongoing commitment to maintaining community benefit contributions and the provision of charitable care, Ascension relies on its strong balance sheet to be able to provide access to care in communities where the operating margins of Ascension hospitals or its other care facilities are often negative. Hospitals that serve higher percentages of uninsured patients and those covered by Medicare and Medicaid are consistently challenged across the sector due to the misalignment of government payment rates to the cost of appropriate care delivery. Our commitment to our Mission calls us to offer healthcare services to these populations despite financial challenges, and our careful stewardship of our resources has supported this priority.
Like any well-run nonprofit organization committed to stewardship, Ascension has a responsibility to operate in a financially sustainable way to, among other things, ensure our associates and clinicians receive fair compensation; pay rapidly rising costs for operating expenses such as supplies, pharmaceuticals and utilities; and maintain and update the advanced medical technology that our clinicians use to save lives and support the health of those we serve.
Our financial reserves (or think of it as “savings”), and the investment returns we earn on those reserves, also enable us to weather known and unknown headwinds and be able to borrow at acceptable interest rates to responsibly fund major capital projects that increase access and enable the effective delivery of care for the benefit of individuals in our communities. This includes maintaining our current inpatient facilities and investing in growing the number and type of both inpatient and outpatient services we offer. Our reserves and investment income also enable us to responsibly fund our pension obligations to many of our long-serving associates. We carefully steward these reserves to ensure our ministry meets communities’ healthcare needs today and is sustainable into the future, all in support of our workforce, patients, and communities we serve.
While a responsible cash reserve for a very large, multistate hospital system has drawn scrutiny, it is notable that our cash on hand decreased almost 30% during the past 18 months. With less cash on hand, our flexibility to respond to crises – like cybersecurity threats or new pandemics – becomes increasingly reliant on debt-based financing and our diminished ability to create returns on investments directly impacts the availability of funds we can dedicate to hospital maintenance, purchasing innovative new equipment, maintaining supplies, and contributing to our communities. Understanding that our operating margins will continue to remain lean for as long as we continue to prioritize caring for the poorest and most vulnerable among us, responsible nonprofit stewardship requires us to maintain reserves that match and support our size and scope.
To that end, even though Ascension experienced an operating loss of $429 million in the three months ending March 31, 2020, the beginning of the pandemic, our cash reserves were crucial and allowed us to quickly provide stability and security for our associates through salary continuation programs and access to care for patients when regular operations – such as elective surgeries, other non-emergency procedures, screenings, and even routine office visits – were suspended or postponed. As has been publicly reported, S&P Global Ratings recently downgraded Ascension’s financial rating from “stable” to “negative” due to “Ascension's multi year trend of operating volatility, coupled with a sizable operating loss in fiscal 2022 and the need to execute on a significant turnaround plan to avoid continued operating losses and weaker cash flow for the rating.” In other words, our reserves represent the difference between a challenged system and a shuttered system. Any implication that Ascension focuses on its bottom line and financial performance for reasons other than supporting our workforce and, most importantly, the patients and communities we serve is belied by these numbers and our demonstrated commitment to associates and patients when COVID-19 hit the United States.
Financial Challenges
Similar to other U.S. healthcare providers, Ascension’s operations and volumes were disrupted by several unexpected COVID-19 surges that created continued volatility for the fiscal year ended June 30, 2022 (FY22). Peaking COVID-19 cases coupled with historic levels of paid staff furloughs due to illness or COVID exposure, rising labor costs, ongoing workforce shortages across the industry, and sporadic closures of surgical and procedural areas, all resulted in very challenging financial performance. For the fiscal year ended June 30, 2022, Ascension sustained an operating loss of nearly $900 million. These challenges have continued into FY23, with an operating loss over the first quarter of the fiscal year of -1.6% following operating margins of -3.4% and -10.0% for the two preceding quarters. These types of losses have impacted healthcare providers across the U.S., even while health insurers continue to earn major profits. Medicare reimbursement rates for hospital services will also not account for these shortfalls; in 2023, Medicare payment rates for inpatient hospitals will increase roughly 2.5% overall, while industry-wide costs have increased roughly 8% year over year. Likewise, Medicaid payment rates continue to significantly under-reimburse for hospital and healthcare services. Our reserves thus often underwrite ongoing losses from patient care services, particularly given that government programs – which comprise significant hospital volume – continue to pay less than the cost of providing the services.
As we have seen during the pandemic, it is in everyone’s interest to have strong and resilient hospitals, as they are the backbone of the entire healthcare system and society’s ultimate safety net. We take care of everyone who walks through our doors 24/7 and invest in the capabilities and resources to strive to maintain round-the-clock hospital services and operations, even in the face of hurricanes and other major disasters. Furthermore, hospitals are often the largest employer in a community. Like many healthcare organizations, Ascension has been able to maintain our stability because of years of responsible saving practices and stewardship of resources – as detailed above – that should be encouraged.
Serving Our Communities
Ascension provides nearly $2.3 billion in care of persons living in poverty and community benefit last year alone. Since fiscal year 2010, Ascension has provided more than $23.5 billion in care of persons living in poverty and community benefit.
In fact, Ascension hospitals serve as the safety-net provider in many communities, providing care for all without regard to their ability to pay. Ascension also operates Dispensary of Hope, a non-profit organization dedicated to providing pharmacies and charitable clinics with reliable access to vital medications at no cost for individuals and families experiencing serious financial challenges. This is possible due to Ascension investment to support Dispensary of Hope and also the generosity of pharmaceutical manufacturers that donate medications to Dispensary of Hope.
In addition, we recently established the Ascension Foundation, a national philanthropic organization that will develop, support and promote activities that advance health equity by supporting novel programs that disrupt generational poverty and create new pathways to economic stability for families and communities, and the creation of a future healthcare workforce that better reflects the race, ethnicity and cultural mix of the country. Learn more by watching this video.
Executive Compensation
Ascension’s unwavering commitment to our Mission, robust community benefit and charitable care offerings, efforts to responsibly steward finite resources, and dedication to our workforce and continuous quality measurement and improvement, are driven by leadership that upholds and demonstrates these values. The Ascension Board of Directors, an independent body, working with a nationally recognized and leading independent compensation consultant, as well as a separate executive compensation committee of the Ascension Board, establishes the organization’s goals and executive compensation to ensure socially responsible and equitable compensation that is competitive and consistent within the healthcare industry as well as among others in our unique space.
Healthcare industry executive compensation programs almost always include financial goals and targets, per industry consultant SullivanCotter. Ascension's executive compensation framework uniquely places a premium on compensation that is “at risk,” with 75 percent tied to Ascension meeting goals related to delivering safe, high-quality care, reducing healthcare disparities, enhancing community health, advancing environmental sustainability, and improving the experience of our patients and our associates. The remaining 25 percent of the at-risk compensation focuses on financial stewardship of the overall health ministry and its Ministry Markets across 19 states accountable for operating performance to ensure the sustainability of our ministry and its Mission to serve all persons, with special attention to those who are poor and vulnerable. While the intense impact of the pandemic has temporarily disrupted this framework, executive compensation decisions still reside with Ascension’s independent Board of Directors and are based on the commitment of leaders to advancing Ascension’s Mission of serving all persons with special attention to those who are poor and vulnerable.
Real Stories About Ascension and Our Caregivers
To better understand the heroic work that our caregivers do every day to serve their communities – especially during the COVID-19 pandemic – visit Ascension Stories. There you will read how:
- Compassion and patience exhibited by the care team at Ascension St. Vincent’s in Florida for a woman suffering from the aftereffects of COVID-19 set the foundation for an overwhelmingly positive experience.
- Collaboration between doctors at Ascension Saint Thomas in Tennessee played a key role in a woman’s journey toward a healthy heart.
- Surgeons at Ascension Via Christi in Kansas teamed up to repair two hernias and remove a cancerous kidney in a single surgery.
- A mom in Florida is grateful that the Neonatal Intensive Care Unit at Studer Family Children’s Hospital at Ascension Sacred Heart was there for her when her two children, born seven years apart, each arrived early.
- A knee replacement performed at an Ascension Illinois hospital is allowing a busy community volunteer and grandmother to stay active, thanks to personalized care and the latest technology.
- Through Ascension Michigan’s compassionate and personalized physical therapy, a woman for whom walking was difficult and sitting was painful regained her quality of life.
- Brain surgery at an Ascension Wisconsin hospital is helping a woman return to a normal life after 14 years of daily seizures.
Any fair story on a health system should include data on workforce, data on quality, data on responsible stewardship, analyses of workforce retention programs, and information about the enormous good the system provides to patients and communities. The New York Times’ series targeting Catholic healthcare has, to date, focused primarily on offering critiques of faith-based systems without recognizing the enormous good that our faith-driven health systems achieve for so many. We are hoping this information presents a fairer picture of Ascension’s commitment to our Mission through our efforts to steadfastly support our caregivers, our patients and our communities.
***
Be sure to learn about some of the heroic work of our caregivers by watching this video.
(1) Data on bedside nursing FTEs was provided to demonstrate clearly that bedside nursing FTEs have been increasing, not decreasing. The Y axis in Table 4 represents bedside nursing FTEs per discharge; “Q1 FY2022” refers to the quarter ending September 30, 2021. The data in Table 4 is specific to nursing FTEs and includes all bedside nurse job categories, which includes RNs, APRNs and LPNs. It does not include CNAs or techs. Within this data, RNs make up 89% of the total. The data reflects care provided across our facilities, including acute care, psychiatric care, rehab, skilled nursing facilities and residential living, long term care hospitals, and other long term subacute care. The data do not include ambulatory care positions. Front-line behavioral health RNs make up 1.45% of the population, while RNs supporting inpatient rehab and long-term care patients make up 0.98% of the nursing FTE population included in this analysis. It is also important to note that the data for FTEs and discharges in this calculation originate from the same facilities (i.e., the same business units and nested departments) in both the numerator and denominator. The discharge data are based on definitions set and adopted across the hospital sector so as not to result in double counting. In order to provide an accurate snapshot of FTEs per discharge, the table we provide (Table 4) displays data on a quarterly cadence. However, the data displayed represent the last month of that quarter – in other words, it is a point-in-time snapshot for each quarter. This represents, then, one month of discharges compared against one month of FTEs. It would be misleading to calculate a ratio of three months’ worth of discharges against one month of FTEs, and a monthly comparison of FTEs against discharges is the standard approach to calculating this metric across all measures of volumes.